Glaucoma Management
Every year, thousands of people are losing their vision. The culprit is an eye disease called glaucoma.
So, what is glaucoma? Glaucoma is the leading cause for irreversible blindness worldwide. Often dubbed as a “silent killer of vision”, it develops without any obvious symptoms in its early stages. By the time the patient has noticed the impairment in their vision, more often than not, it would already have been too late. In fact, as much as 40% of the vision can be lost without the patient noticing it! This condition has been projected to increase 101% by 2040 in a Singapore consensus study.
What is Glaucoma?

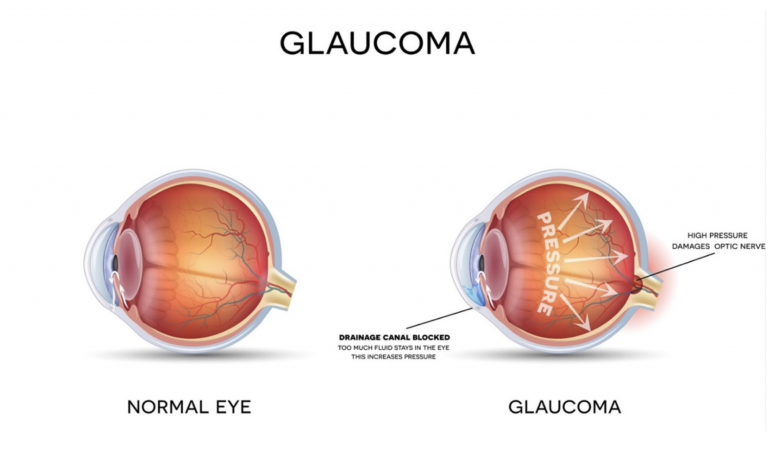
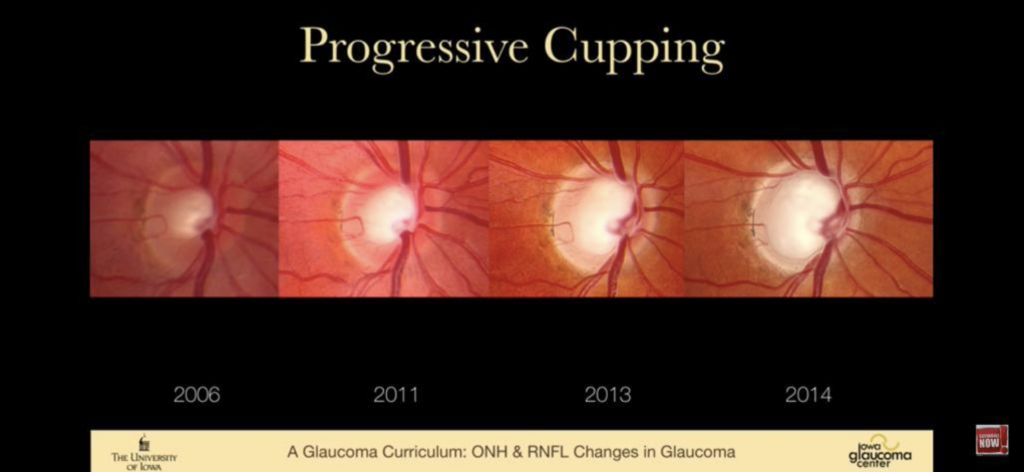
Glaucoma is a condition where the nerve of the eye, called the optic nerve, is damaged. The damage progresses with time and is irreversible. There are many causes that damage the optic nerve. The most common being a build up of pressure in the eyeball because the fluid is unable to drain efficiently.

A good analogy will be to compare the eye to the air pressure of a car tyre. Just as a tyre needs a specific amount of air pressure to retain its shape and stay firm, the eyeball requires the correct amount of Intra-Ocular Pressure (IOP) to be able to function properly. When there is an increase in eye pressure which cannot be relieved, the prolonged elevated pressure continues to push against the optic nerve causing damage. This process is irreversible, and so is the vision loss.
If left untreated, this eye condition will lead to diminished visual field (particularly in the peripheral line of sight) and eventually, blindness will creep in.
What are the different types of Glaucoma?
In general, there are 5 different types of glaucoma, which is caused by a number of different factors:
1. Primary Open-Angle Glaucoma
The most common form of glaucoma, open-angle glaucoma, usually has no symptoms prior to advanced peripheral vision loss. When significant visual field loss occurs, one may experience patchy vision or blind spot. However, the irreparable damage and vision loss may be so slow that it goes unrecognised before any symptoms become apparent.
2. Chronic Angle-Closure Glaucoma & Acute Angle-Closure Glaucoma
Another common form of glaucoma in Asians is angle-closure Glaucoma. In acute angle-closure glaucoma, the flow of the fluid in the eye, called aqueous humor, is suddenly blocked. This causes a rapid build-up of fluid in the eye and thus, causing very high Intra-Ocular Pressure. If you experience sudden symptoms such as severe eye pain, one-sided headache, nausea, together with eye redness and blurred vision, you should see your eye specialist immediately. The chronic angle-closure glaucoma, like open-angle glaucoma, has no symptoms prior to advanced peripheral vision loss.
3. Normal Tension Glaucoma
It may come as a surprise to you, but patients without increased Intra-Ocular Pressure may also sustain damage to their optic nerves. The mechanism is not well understood. Recent scientific studies suggest that it might be associated with increased risk of neurodegenerative conditions such as Alzheimer’s Disease or Dementia.
4. Secondary Glaucoma
Secondary glaucoma is caused by other existing medical conditions, leading to an elevated level of eye pressure. For instance, serious eye trauma and inflammation, poorly controlled diabetes, tumour, cataract or retinal blood vessel blockage can lead to this condition, resulting in optic nerve damage and vision loss. For patients with secondary glaucoma, treatment must address both the elevated IOP and the underlying medical cause.
5. Congenital and Juvenile Glaucoma
Though it is uncommon, but it is possible for infants and children to develop glaucoma. In this case, the damage of optic nerves can result from the slow or blockage in the eye aqueous drainage or an underlying medical condition. Congenital glaucoma are hereditary and can be passed down through the abnormal recessive genes.
How do I recognise the symptoms of Glaucoma?
Recognising glaucoma in the early stages can be tricky but vital. Since it often has no apparent symptoms prior to significant peripheral vision loss, many glaucoma patients are unaware that they are suffering from this disease. The vision loss is so gradual that you may not even notice it until the condition is at an advanced stage.
If you experience any of the following symptoms, you should seek immediate help:
- Loss of peripheral or side vision (this is usually the first sign of glaucoma)
- Eye redness
- Increased sensitivity to lights
- Appearance of halos (rainbow-coloured) around bright lights
- Blurry or foggy vision
- Sudden sight loss
- Cloudy-looking cornea
- Nausea and vomiting (accompanying severe eye pain)

As you may have noticed, these are symptoms common to many other eye diseases. They can easily be missed out or brushed off as other “not-as-serious” eye problems. Given the silent nature of glaucoma, we would urge our patients/ readers to undergo regular eye checks which allows early detection and intervention of the disease.
Am I at risk of Glaucoma?

Generally, the risk of glaucoma increases with age. Although the most common form of glaucoma affects mostly people above 60 years old, you should not let your guard down as it can affect people of all ages. Other risk factors of this eye disease include:
- Family history of glaucoma
- Having high internal eye pressure (Intra-Ocular Pressure)
- Thin cornea
- High myopia (severe near-sightedness)
- Previous eye injury
- Being diagnosed with other certain medical conditions, such as diabetes, heart disease, high blood pressure, etc
What can I do to prevent or lower my risk of Glaucoma?
While there are no known ways to prevent glaucoma entirely, blindness or significant vision loss could be avoided if the disease is recognised in the early stages. This is why if you belong to either of the above higher risk groups, we will strongly recommend you to see an eye doctor for a regular comprehensive eye exam. Your eye doctor will tell you how often to have follow-up exams based on the results of this eye health screening.
Nonetheless, medical experts recommend a healthy lifestyle for those who are at risk of developing glaucoma, such as to:
- Maintain a healthy weight
- Keep the eye pressure in check
- Include exercise in the daily routine
- Prevent overexposure to sunlight by wearing sunglasses or hats when outdoors
- Limit caffeine intake to moderate levels
- Avoid smoking
- Eating a well-balanced diet, including “vision foods” to support your eye health such as lutein and zeaxanthin (e.g. spinach, kale, etc), vitamin A (carrots, egg yolks, etc), omega-3 fatty acids (salmon, chia seeds, etc)
- Control other medical conditions which may give rise to glaucoma (if any). For instance, high blood pressure can be prevented or managed by simply making positive lifestyle changes and taking medications if needed.
There is a silver lining in all of this. Other than being able to slow down the progression of glaucoma, you will be able to enjoy a vibrant, active life with a healthy body and a healthy mind. Remember, making gradual small changes to your daily lifestyle can go a long way.
I have been diagnosed with Glaucoma – now what?
While there is no cure for glaucoma at this point of writing, there are several ways to slow down glaucoma progression.
The goal of glaucoma treatment is to lower the Intra-Ocular Pressure (IOP) to an acceptable range, thus reducing damage to the optic nerves. What one has got to bear in mind is that glaucoma treatment is a lifelong process and must be continued throughout life, and that any vision loss is permanent and irreversible.
Depending on the type of glaucoma, there are three types of management options, which can be classified into:
- Medical Treatment
- Surgical (Incisional) Treatment
- Laser Treatment

Medical Treatment
This is the most common form of glaucoma treatment. It comes in the form of eye drops regime but can also come in the form of intravenous or oral anti-glaucoma medications, especially for the acute glaucoma attack.
Pros
Requires high level of patients’ compliance.
Cons
Some side-effects may be experienced.
Surgical (Incisional) Treatment
This is usually administered if medical therapy fails. The most common form is trabeculectomy, where the surgeon will make a cut in the eye, creating an outflow channel for the eye aqueous fluid into the surrounding eye tissue, thus significantly reducing Intra-Ocular Pressure.
A newer type of surgery termed Minimally-invasive Glaucoma Surgery (MIGS) involves using micro-implants in the form of stents or shunts to achieve significant reduction of Intra-Ocular Pressure with lower surgery risks and downtime.
Pros
Effective even for patients with severe glaucoma. Minimally-invasive procedures with a good safety profile, especially in the short-to-medium term
Cons
Carry surgical risks, particularly for the larger incisional procedures
Laser Treatment
Laser treatment can be carried out in patients with angle-closure glaucoma (laser iridotomy, laser iridoplasty) or in patients with open-angle glaucoma (Selective laser trabeculoplasty (SLT)). SLT has become an evidence-based first-line treatment for open-angle glaucoma, especially for patients who cannot tolerate or are not compliant to medical treatment.
Pros
Lasers are non-invasive procedures with good safety profile.
Cons
Less IOP reduction as compared to conventional glaucoma surgeries, more suitable only for patients with mild to moderate glaucoma.
Can I use my Medisave to pay for my Glaucoma treatments?
Unfortunately, glaucoma medications are not Medisave-claimable.
In Conclusion
Love your eyes? One of that you can protect your vision is by undergoing your regular comprehensive eye checks. Glaucoma cannot be self-detected. This is the only way you can make sure that this silent disease can be diagnosed early and nipped in the bud as early as possible.
According to the American Academy of Ophthalmology, these are the recommended intervals for eye exams:
- Age 20 to 29: Every 3 to 5 years for individuals at high risk or with a family history of glaucoma. Others should have an eye exam at least once during this period.
- Age 30 to 39: Every 3 to 5 years for individuals at high risk or with a family history of glaucoma. Others should have an eye exam at least twice during this period.
- Age 40 to 64: Every 2 to 4 years.
- Age 65 or older: Every 1 to 2 years.
If you would like to book your comprehensive glaucoma screening with us,
📞 Call us at 6733 3316
📱 WhatsApp us at 8383 7989
✉️ Email us at doctor@clearvision.com.sg
🤳 Message us on Facebook
🤳 Message us on Instagram
The glaucoma screening costs $380 and will take around 1 – 2 hours.
It will include a series of eye tests as well as a personal consultation with your lasik surgeon.

